"Better Than Medication" Improving VO2max and Lowering ApoB in 12 Weeks
“Your exercise is better than medication.”
— Client's Primary Care Physician
This is the feedback “Dave” (a pseudonym) received from his doctor after 12 weeks of aerobic training aimed at improving his VO2max.
Below, we will outline the specific training protocols Dave used to improve his VO2max by over 15% and significantly lower his cholesterol— and specifically lowering ApoB— allowing him to avoid the statins his cardiologist had originally suggested.
First, we will review Dave's background and his physiological starting point, then detail the programming that led to these results.
Dave performed an EKG stress test and VO2max in my San Diego laboratory.
Description of Case
Subject Profile: 67-year-old male, retired.
Dave initially approached me specifically for a VO2max test. A combination of family history, concerning blood work, and a coronary calcium score had motivated him to improve his metabolic health through lifestyle changes rather than pharmacology.
While his cardiologist had suggested a statin protocol, Dave has a severe lactose allergy (a common filler in some medications) and preferred a lifestyle-first approach.
He is also data-driven; he consumes content from longevity experts and utilizes both an Apple Watch and Oura Ring. He wanted coaching that integrated his metabolic test results with his daily wearable data.
The Starting Point
Dave was not “unhealthy” by standard metrics; he was looking to optimize. Despite a genetic predisposition to cardiovascular disease, he maintained a normal body composition and was already proactive, working with a dietician and a strength coach.
Our initial VO2max test placed him in the borderline "Good to Excellent" range for his age group. His goal was to move beyond this into the "Superior" category.
Results: Biometrics & Performance
Within eight weeks, Dave’s lowest observed resting heart rate dropped from 50 bpm to 46 bpm.
By month four, we consistently observed 44 bpm.
Dave’s actual RHR data
By week 12, his HRV (RMSSD) sustained values in the upper 30s while maintaining a high training load, and mid-40s by 5 months.
HRV from his Oura Ring
This is a critical distinction: high HRV often results from cessation of training (recovery), but maintaining high HRV during training indicates improved autonomic adaptation.
At the 12-week mark, we re-tested his VO2max. The improvement was significant enough that we had to alter the test protocol mid-test to accommodate his new fitness level.
Result: A 6.7 mL/kg/min increase in VO2max. A >15% increase!
Classification: Moved from "Good/Excellent" border to "Excellent/Superior" border.
Results: Blood Work
Perhaps the most compelling data came from Dave’s lipid panel.
Note: Dave had been consuming niacin, psyllium, and plant sterols during this period, which contributed to these improvements.
However, his physicians noted that the magnitude of change exceeded what is typically seen with supplements alone.
Pre-Training —> Post-Training
Triglycerides: 48 —> 38
LDL: 110 —> 71
HDL: 48 —> 61
ApoB: 94 —> 71
Total Cholesterol: 210 —> 158
Training Methodology
We built Dave's programming around a 3-zone heart rate model derived specifically from his metabolic thresholds (VT1 and VT2), rather than the standard 5-zone model used by fitness watches.
While 5-zone models are useful for general fitness, a 3-zone model allows us to prescribe exercise based on real physiological markers:
Zone 1: Below VT1 (Moderate Domain)
Zone 2: Between VT1 and VT2 (Heavy Domain)
Zone 3: Above VT2 (Severe Domain)
We focused on finding a sustainable volume limit with a large bias toward low-intensity work. Once we established a consistent schedule, we slowly introduced intensity.
Time and time again, research shows that personalized threshold-based exercise prescription fares better than standard programming.
Percent time spent in HR zones and aerobic training time. Colors are time distribution in each zone, while the blue line is monthly total aerobic training hours.
Exercise Selection
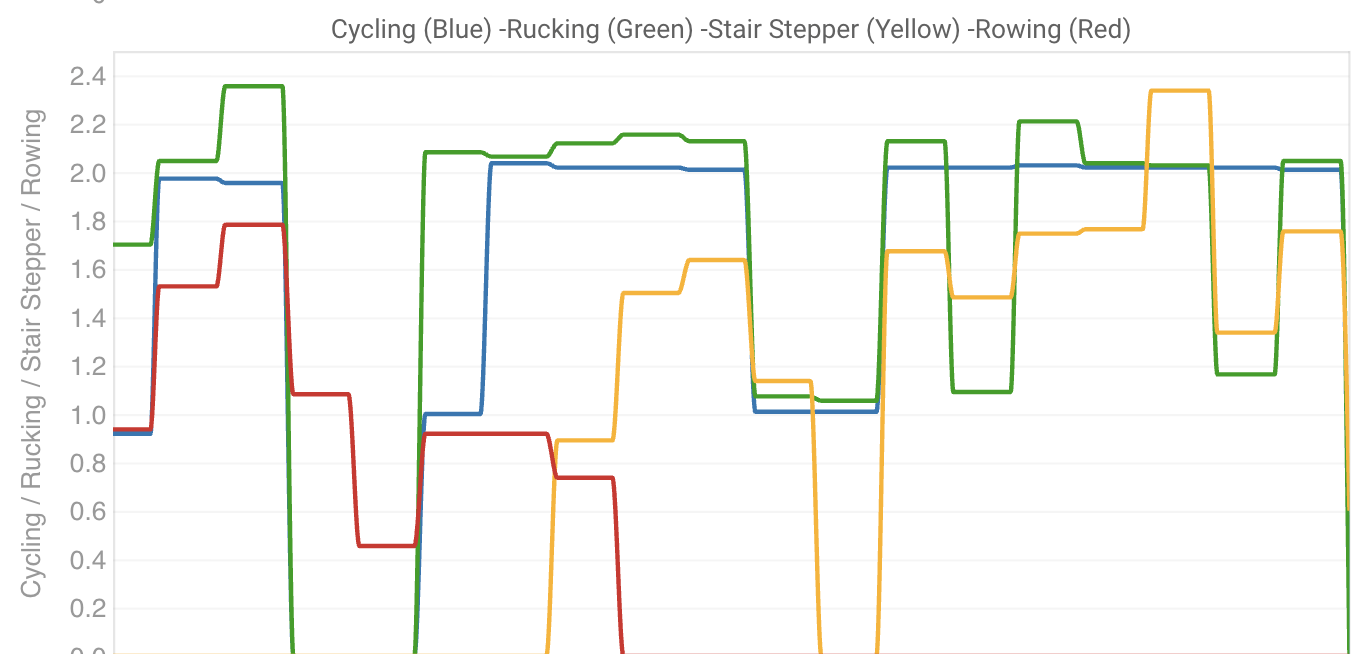
We selected activities based on Dave’s preferences and their ability to generate the necessary cardiac output. This included rucking, cycling, and eventually, the Stairmaster.
Initially, we programmed rowing for his high-aerobic intervals. However, we found that rowing failed to elicit the oxygen uptake required for VO2max improvement.
In some cases*, rowing is technically demanding and often limited by muscular fatigue in the smaller muscle groups (upper body) before the cardiovascular system reaches its limit.
To drive VO2max, we need to recruit maximum muscle mass to demand maximum oxygen. We pivoted to the Stairmaster, which utilized his lower body musculature to drive his heart rate up without technical limitations.
Rowing is a fantastic exercise but for this specific case, we needed an alternative.
Here’s an example of a stairmaster workout we used often.
As Dave adapted, we monitored his biometrics (Sleep, Resting Heart Rate and HRV) to ensure the stress was appropriate. Once we saw positive adaptation, we increased the intensity, adding VO2max intervals on the Stairmaster and respiratory training at the end of low-aerobic sessions.
Weekly time spent with each type of exercise.
Progress & Summary
These changes were achieved with 4 to 6 hours of dedicated aerobic work per week, alongside his strength training and yoga.
While the physiology is complex, the execution was simple: Dave put in the work. He rarely missed a session and adhered strictly to the prescribed intensities.
Dave’s results are a product of precision, not magic. If you are collecting data with a Garmin, Apple Watch or Oura Ring but aren't seeing the health metrics to match, you likely need a plan customized to your physiology.
If you are interested in moving your health from "normal" to "superior," please reach out to schedule a consultation or fill out this training application.